Inflammation is a key indicator in biopsy reports, often holding the key to understanding your health. As you delve into your biopsy results, recognizing the nuances of inflammation can empower you to engage actively with your healthcare decisions.
What You Will Learn
- Inflammation is a protective response of the immune system to injury or infection, crucial for healing.
- Acute inflammation is short-term and resolves quickly, while chronic inflammation can last for months or years, potentially leading to complications.
- Understanding the types of inflammation—acute, chronic, and focal—can help in interpreting biopsy results accurately.
- Inflammation can obscure other important findings in biopsy samples, making follow-up tests essential for accurate diagnosis.
- Engaging in open dialogue with your healthcare provider about inflammation findings can enhance your treatment approach and management strategies.
Understanding Inflammation Types and Their Impact in Biopsy Reports
This visual summarizes the key characteristics, cellular involvement, and implications of acute and chronic inflammation frequently found in biopsy results.
Acute Inflammation
Characteristics: Rapid onset, short duration. Resolves once cause is addressed.
Cellular Involvement: Predominantly neutrophils and plasma proteins.
Implications: Active healing process or ongoing infection.
Chronic Inflammation
Characteristics: Prolonged response (months/years), persistent.
Cellular Involvement: Lymphocytes, macrophages, and plasma cells.
Implications: Potential for tissue damage, disease progression.
Common Causes
- Infection: Bacteria, viruses, fungi.
- Autoimmune Diseases: Body attacks healthy tissues.
- Malignancy: Tumors create inflammatory microenvironment.
- Necrosis: Tissue death from injury or lack of blood supply.
Interpretive Challenges
- Impact on Diagnosis: Can obscure other significant findings.
- False Negatives: Risk of misdiagnosis due to inflammation.
- Additional Tests: Often required for clarity (blood, imaging, repeat biopsies).
- Histopathology: Essential for microscopic cellular analysis.
Understanding Inflammation in Biopsy Reports
When we think about biopsy reports, one term that frequently appears is inflammation. But what does it truly mean, and why is it significant? Inflammation is a natural response of your body to injury or infection, playing a crucial role in the healing process. However, understanding inflammation within the context of biopsy results can feel overwhelming. At What Is A Biopsy, my goal is to simplify this information, helping you navigate your health with confidence.
Inflammation can manifest in various ways in biopsy samples, each providing insights into your body's response to different challenges. Understanding the distinctions between types of inflammation, their causes, and their implications can empower you to have informed discussions with your healthcare provider.
What is Inflammation in Biopsy Results?
To begin, let’s define inflammation and its role in tissue response. Essentially, inflammation is a defensive reaction initiated by your immune system in response to harmful stimuli, such as pathogens or damaged cells. This response involves various immune cells and biochemical processes aimed at restoring tissue integrity. While this is a protective mechanism, it can also lead to persistent problems if the inflammation becomes chronic.
- Definition of Inflammation: A protective bodily response to injury or infection.
- Role of Inflammation: Helps in healing but can lead to complications if unresolved.
- Chronic Inflammation: When inflammation persists and may cause additional health issues.
Understanding these terms is vital for interpreting biopsy results accurately. You might encounter terms like acute or chronic inflammation, each indicating different timelines and implications for your health.
Defining Inflammation and Its Role in Tissue Response
Inflammation is not just a single event; it is a complex process involving various cellular players. The body's defense mechanism sends out signals to alert immune cells, which rush to the affected area. This is why inflammation can lead to symptoms like swelling, redness, and pain as your body works to heal itself.
In biopsies, these reactions can provide vital clues about what is happening in the tissue. By understanding how inflammation works, we can better interpret its significance in your biopsy results, making it easier for you to understand what your report means.
Common Terms Explained: Acute vs. Chronic Inflammation
Let’s clarify two key terms you may see in your biopsy report: acute and chronic inflammation. Acute inflammation is a short-term response, often noticeable through symptoms like pain and swelling, typically resolving once the underlying cause is addressed. In contrast, chronic inflammation can persist for months or years, sometimes leading to tissue damage and other serious health conditions.
- Acute Inflammation: Rapid onset, often resolving quickly.
- Chronic Inflammation: Long-lasting, potentially causing further complications.
Recognizing the difference between these two types of inflammation can enhance your understanding of your health and the treatments your doctor may recommend.
Types of Inflammation Detected in Biopsy Samples
In biopsy samples, different types of inflammation can be identified, each with unique characteristics. Let's explore these types and their significance. Understanding these distinctions can help you and your healthcare provider better assess your overall health.
Acute Inflammation: Key Characteristics and Cellular Involvement
Acute inflammation is characterized by a rapid onset and a short duration. During this process, your body sends white blood cells, especially neutrophils, to the affected area. These cells help combat infection and facilitate healing. In biopsy samples, you might see signs of acute inflammation such as increased blood flow and the presence of these immune cells.
- Key Characteristics: Redness, heat, swelling, and pain.
- Cellular Involvement: Predominantly neutrophils and plasma proteins.
Recognizing these characteristics in your biopsy results can indicate an active healing process or an ongoing infection.
Chronic Inflammation: Implications and Cellular Composition
Chronic inflammation, on the other hand, can signal a more complex issue. In this case, the immune response is prolonged, often with a different cellular makeup. Instead of primarily neutrophils, you might see lymphocytes and macrophages, indicating a persistent inflammatory process. This type of inflammation can be a factor in conditions like long-term low-grade intestinal inflammation, which may be prevalent among patients who have undergone radiotherapy, as highlighted in some research (Source: ASCO Post).
- Implications: Potential for tissue damage and disease progression.
- Cellular Composition: Lymphocytes, macrophages, and plasma cells.
Understanding chronic inflammation's implications can help guide treatment decisions moving forward.
Focal Inflammation: Understanding Its Unique Characteristics
Focal inflammation refers to inflammation that is limited to a specific area of tissue. This localized response is critical to understand, as it can indicate a specific problem or injury to a tissue rather than a systemic issue. In biopsy reports, focal inflammation may suggest the need for targeted treatment.
- Characteristics: Localized swelling and immune response.
- Clinical Significance: May indicate targeted treatment is necessary.
Identifying focal inflammation can lead to more precise diagnoses and tailored treatment plans.
Causes of Inflammation Found in Biopsy Samples
Understanding the causes of inflammation detected in biopsy samples is essential for better patient care. Let's discuss some common causes that can lead to inflammation and what they mean for your health.
Infection: Understanding Pathogens and Immune Response
One of the most common causes of inflammation is infection. When pathogens such as bacteria, viruses, or fungi invade the body, your immune system responds by initiating inflammation to fight off the invaders. This can lead to noticeable symptoms and is often reflected in biopsy results.
- Bacterial infections
- Viral infections
- Fungal infections
Recognizing infection as a cause of inflammation helps inform the appropriate treatment options, whether it's antibiotics or supportive care.
Autoimmune Diseases: When the Body Attacks Itself
Another important factor in inflammation is autoimmune diseases. In these conditions, the immune system mistakenly attacks healthy tissues, leading to chronic inflammation. Examples include rheumatoid arthritis and lupus, both of which can significantly impact your health.
- Examples: Rheumatoid arthritis, lupus, and multiple sclerosis.
Understanding autoimmune diseases in relation to inflammation can enhance communication with your healthcare team and help you manage your condition effectively.
Malignancy: The Tumor Microenvironment and Inflammation
Inflammation can also be associated with malignancy. Cancerous tumors can create a microenvironment that fosters inflammation, potentially leading to a cycle of growth and invasion. For instance, the role of inflammation in cancer progression and response to therapy is a growing field of study (Source: Nature Communications). Identifying inflammation in the context of tumors is critical for diagnosis and treatment planning.
- Connection: Tumors can elicit an inflammatory response.
- Clinical Relevance: Inflammation can indicate tumor aggressiveness.
Understanding this connection can lead to more comprehensive care as you navigate your treatment options.
Other Factors: Necrosis and its Role in Inflammatory Response
Furthermore, necrosis, or tissue death, can trigger inflammation. When cells die from injury or lack of blood supply, the body responds with inflammation to clear away dead tissue and promote healing. This can be a significant factor in various conditions, making it important to recognize in biopsy reports.
- Examples of Causes: Trauma, ischemia, and certain diseases.
By understanding how necrosis contributes to inflammation, you can better appreciate the findings in your biopsy report.
Common Conditions Associated with Chronic Inflammation: From Rheumatoid Arthritis to Inflammatory Bowel Disease
Several conditions are linked to chronic inflammation, including rheumatoid arthritis and inflammatory bowel disease (IBD). These diseases can lead to long-term health implications, and understanding their connection to inflammation is crucial for effective management.
- Rheumatoid Arthritis: Affects joints and causes chronic pain.
- Inflammatory Bowel Disease: Includes Crohn's disease and ulcerative colitis.
Recognizing these conditions can help foster a more productive conversation with your healthcare provider about your care options.
Interpreting Inflammation in Biopsy Results
Interpreting the results of your biopsy requires a thorough understanding of inflammation. Let’s explore how inflammation affects the interpretation of your biopsy results.
How Inflammation Affects Biopsy Interpretation
Inflammation can significantly influence how pathologists interpret biopsy samples. When inflammation is present, it can obscure other findings, making it challenging to accurately diagnose underlying conditions. This is why understanding the context of inflammation in your results is so important.
- Impact on Diagnosis: Inflammation may mask malignancies or other issues.
- Importance of Context: The cause and duration of inflammation matter.
Recognizing these factors can help you better understand your biopsy results and what they mean for your health moving forward.
False Negatives: The Risk of Misdiagnosis in Inflamed Tissue
One significant risk associated with inflammation in biopsy samples is the potential for false negatives. Inflammation can lead to misinterpretation, causing pathologists to overlook serious conditions. Being aware of this risk can help you advocate for more thorough evaluations if necessary.
- Potential for Misdiagnosis: Inflammation can obscure important findings.
- Importance of Follow-Up: If something seems off, don’t hesitate to ask for further testing.
Understanding this aspect of inflammation can help you stay proactive in your healthcare journey.
Essential Role of Additional Diagnostic Tests
Given the complexities involved, additional diagnostic tests may be necessary to clarify findings in inflamed tissue. Tests such as blood work, imaging, or repeat biopsies can provide valuable information to ensure an accurate diagnosis. This may seem daunting, but these steps can provide clarity and peace of mind. For example, some studies discuss the diagnostic challenges of inflammation, particularly in the context of specific conditions like sarcoidosis of the prostate, where inflammation can mimic malignancy (Source: PMC NCBI).
- Types of Additional Tests: Blood tests, imaging studies, and follow-up biopsies.
- Why They Matter: They can confirm or rule out serious conditions.
Being informed about these tests can help you feel more in control of your healthcare decisions.
Understanding Histopathology and Its Relevance to Inflammation
Finally, histopathology plays a crucial role in understanding inflammation in biopsy results. This branch of pathology focuses on examining tissue samples under a microscope to identify cellular changes and characteristics. By studying these samples, pathologists can glean invaluable insights into the nature of the inflammation and any underlying conditions.
- Key Focus: Cellular structure and composition in inflamed tissue.
- Clinical Relevance: Helps in diagnosing conditions accurately.
Gaining an understanding of histopathology can empower you to ask informed questions during discussions with your healthcare provider.
Clinical Significance of Inflammation Findings
The findings related to inflammation in your biopsy report hold significant clinical importance. Understanding these implications can guide your treatment journey and improve your overall care.
How Inflammation Impacts Diagnosis and Prognosis
Inflammation can influence both diagnosis and prognosis. If your biopsy shows significant inflammation, it may suggest an active disease process or a response to treatment. This information can help your healthcare team devise a tailored approach to your care.
- Diagnosis Impact: May signal the need for additional tests or treatments.
- Prognosis Insight: Helps assess the severity of your condition.
Understanding how inflammation affects your diagnosis can lead to more personalized care.
Inflammation's Influence on Treatment Decisions and Patient Management
Furthermore, inflammation plays a crucial role in treatment decisions. Depending on the findings in your biopsy report, your doctor may recommend specific medications or therapies aimed at reducing inflammation. This can be particularly important in managing autoimmune diseases or chronic conditions.
- Potential Treatment Options: Corticosteroids, immunosuppressants, or targeted therapies.
- Management Strategies: Lifestyle changes and ongoing monitoring.
Recognizing how inflammation informs treatment can help you feel more engaged in your care plan.
Exploring Treatment Options for Inflammation: Corticosteroids and Immunosuppressants
Several treatment options exist to manage inflammation. Medications like corticosteroids and immunosuppressants can help reduce inflammation and its effects on your body. Understanding these options can empower you in your treatment decisions.
- Corticosteroids: Help reduce inflammation quickly.
- Immunosuppressants: Target the immune response to decrease inflammation.
Being informed about your treatment options can foster a sense of confidence as you work with your healthcare team.
Communicating Inflammation Results with Healthcare Providers
When it comes to your biopsy results, clear communication with your healthcare provider is essential. Let’s explore how to effectively discuss inflammation findings.
Understanding Your Pathology Report: Key Points to Discuss
Your pathology report can be complex, but certain key points can help make discussions with your doctor more productive. Focus on understanding the significance of inflammation in your report and how it relates to your overall health.
- What to Ask: What does the inflammation mean for my diagnosis?
- Key Points: Any recommended follow-up tests or treatments based on this finding.
Being prepared with these questions can make your conversations with your healthcare team more meaningful.

Questions to Ask Your Doctor About Inflammation Findings
Don’t hesitate to ask questions during your appointments! This is crucial for your understanding and peace of mind. Consider asking about treatment options, lifestyle changes, or anything else that comes to mind.
- Suggested Questions: What is the next step based on my inflammation findings?
- Further Inquiries: How can I manage my condition effectively?
Asking questions fosters open dialogue, ensuring you feel supported throughout your healthcare journey.
Importance of Medical History and Symptoms in Inflammation Assessment
Your medical history and symptoms play a critical role in assessing inflammation. Sharing these details with your healthcare provider can help them make accurate diagnoses and treatment plans tailored to your needs.
- History Matters: Previous health issues can influence current inflammation.
- Symptom Tracking: Keeping a record of your symptoms can aid in discussions with your doctor.
Being proactive about your medical history can enhance the quality of care you receive.
Frequently Asked Questions (FAQs) About Inflammation in Biopsy Reports
- Q1: What is inflammation in the context of a biopsy report?
- A1: Inflammation is your body's natural protective response to injury, infection, or irritation. In a biopsy report, it indicates the presence of immune cells and biochemical processes attempting to heal damaged tissue or fight off pathogens.
- Q2: What is the difference between acute and chronic inflammation?
- A2: Acute inflammation is a rapid, short-term response (e.g., from an infection or injury), characterized by cells like neutrophils. Chronic inflammation is a prolonged response (months to years) involving different immune cells like lymphocytes and macrophages, and can lead to tissue damage.
- Q3: Can inflammation in a biopsy report obscure other important findings?
- A3: Yes, inflammation can sometimes mask or complicate the diagnosis of other conditions, including malignancy, potentially leading to false negatives. This often necessitates additional diagnostic tests.
- Q4: What are the common causes of inflammation found in biopsy samples?
- A4: Common causes include infections (bacterial, viral, fungal), autoimmune diseases (where the body attacks its own tissues), malignancy (tumors creating an inflammatory microenvironment), and necrosis (tissue death).
- Q5: What should I do if my biopsy report shows inflammation?
- A5: You should discuss the results thoroughly with your healthcare provider. Be prepared to ask questions about the type of inflammation, its potential causes, whether additional tests are needed, and how it impacts your diagnosis and treatment plan.
Visual Aids and Resources for Better Understanding
Visual aids can be incredibly helpful in understanding the inflammation discussed in your biopsy results. Let’s explore some resources that can enhance your knowledge.
Infographics on Inflammation Types and Biopsy Interpretation
Infographics can provide a clear visual representation of different types of inflammation and their implications. These resources can simplify complex information, making it easier to grasp.
- Benefits of Infographics: Simplifies understanding and enhances retention.
- Where to Find: Websites like What Is A Biopsy may offer valuable infographics.
Visualizing the information can make discussions with your healthcare team more productive.
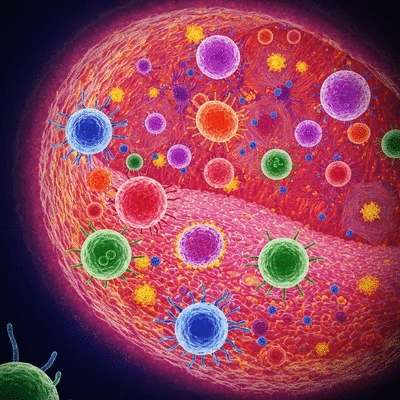
Microscopy Images: Visualizing Inflammatory Cells
Microscopy images can offer a fascinating glimpse into the cellular components of inflammation. By seeing these images, you can better appreciate the cellular activity that occurs during inflammation and its relevance to your biopsy results.
- Understanding Microscopy: Provides insight into the types of cells involved.
- Application: Useful when discussing results with your healthcare provider.
Utilizing these images can empower you with knowledge about your health.
Pro Tip
When discussing your biopsy results with your healthcare provider, consider bringing along a list of specific questions. This can include inquiries about the implications of inflammation, potential follow-up tests, and treatment options. Being prepared not only aids your understanding but also empowers you to take an active role in your health care journey.
Next Steps After Receiving Inflammation Results
Receiving your biopsy results can be overwhelming, especially when inflammation is detected. It's essential to know what your next steps should be, as this information plays a significant role in your health journey. Here are some actions to consider after getting your inflammation results:
Follow-Up Actions: What Should Patients Do?
It's crucial to approach your situation with a proactive mindset! Here are some follow-up actions you might consider:
- Discuss your results with your healthcare provider: Schedule a meeting to go through the results in detail.
- Consider additional testing: If your doctor recommends it, be open to further tests or repeat biopsies to get a clearer picture.
- Monitor your symptoms: Keep track of any changes in your body or health, and report these to your doctor.
Communication is key! Being informed will help you understand the potential implications of your inflammation results. Don’t hesitate to ask questions about your health, treatment options, or concerns you might have.
When to Consider Additional Testing or Repeat Biopsies
Sometimes, inflammation in biopsy results can necessitate additional testing. Here are some scenarios when this might be needed:
- If initial test results are inconclusive
- When your symptoms change or worsen
- If there's a need to monitor a chronic condition
Being vigilant about your health can make a big difference! I encourage my patients to stay engaged with their healthcare process.
Importance of Monitoring and Ongoing Evaluation
Following up on inflammation findings is vital for your overall health management. Regular evaluations can help:
- Track the progression or improvement of inflammation
- Adjust treatment plans as necessary
- Identify potential complications early
Think of this ongoing evaluation as a vital part of your health journey. Staying connected to your healthcare team will empower you and ensure you receive the right support.
Addressing Secondary Infections and Associated Risks
Inflammation can sometimes lead to secondary infections, which adds complexity to your situation. It's important to be aware of the signs of infections, such as:
- Fever or chills
- Increased swelling or redness at the biopsy site
- Unusual discharge or drainage
If you notice any of these symptoms, contact your healthcare provider immediately! Early intervention can prevent complications and improve your recovery experience.
Summary of Inflammation Implications in Biopsy Reports
Understanding the implications of inflammation found in your biopsy report is crucial for effective patient care. Here are some key takeaways:
- Inflammation can signal a variety of underlying conditions, requiring careful monitoring.
- Engaging in open dialogue with your healthcare provider can clarify uncertainties and foster better treatment plans.
- Your health journey is a partnership; be active in discussions about your care and treatment options.
Remember, staying informed and involved in your healthcare decisions is empowering. As a pathologist, I always emphasize the importance of clear communication in navigating these complex situations.
Encouraging Open Dialogue with Healthcare Providers
Effective communication with your healthcare team is essential! Don't hesitate to share your concerns or ask questions about your biopsy results. Here are some questions you might consider asking:
- What do my inflammation results mean for my diagnosis?
- What are the next steps in my treatment plan?
- How can I best monitor my symptoms and health moving forward?
By fostering an open dialogue, you can enhance your understanding and contribute to more personalized care!
Resources for Further Learning and Support
At What Is A Biopsy, we believe that knowledge is empowerment! Here are some great resources that can help you better understand inflammation and biopsy:
Patient Education Materials on Inflammation and Biopsy
Our website offers a variety of educational articles and animations specifically designed to explain the nuances of biopsy procedures and interpretations. These resources are doctor-reviewed and are intended to demystify the biopsy process.
Support Groups and Online Communities for Patients
Connecting with others who share similar experiences can be incredibly supportive. Look for local or online support groups where you can share your thoughts and gain insights from others.
Research Studies on Inflammation and Its Treatment Options
Staying informed about the latest research can be beneficial. There are numerous studies that explore inflammation's role in different health conditions, and understanding these can help you navigate your treatment options more effectively.
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Inflammation is a natural protective response to injury or infection, but understanding its implications in biopsy results is crucial.
- Acute inflammation is short-term and can resolve quickly, whereas chronic inflammation can lead to serious health complications.
- Different types of inflammation (acute, chronic, focal) provide insights into tissue response and potential underlying issues.
- Inflammation can mask other conditions in biopsy results, making accurate interpretation essential for diagnosis.
- Effective communication with healthcare providers about inflammation findings is vital for informed treatment decisions and patient management.